Glaucoma Specialist San Diego, CA
What is Glaucoma?
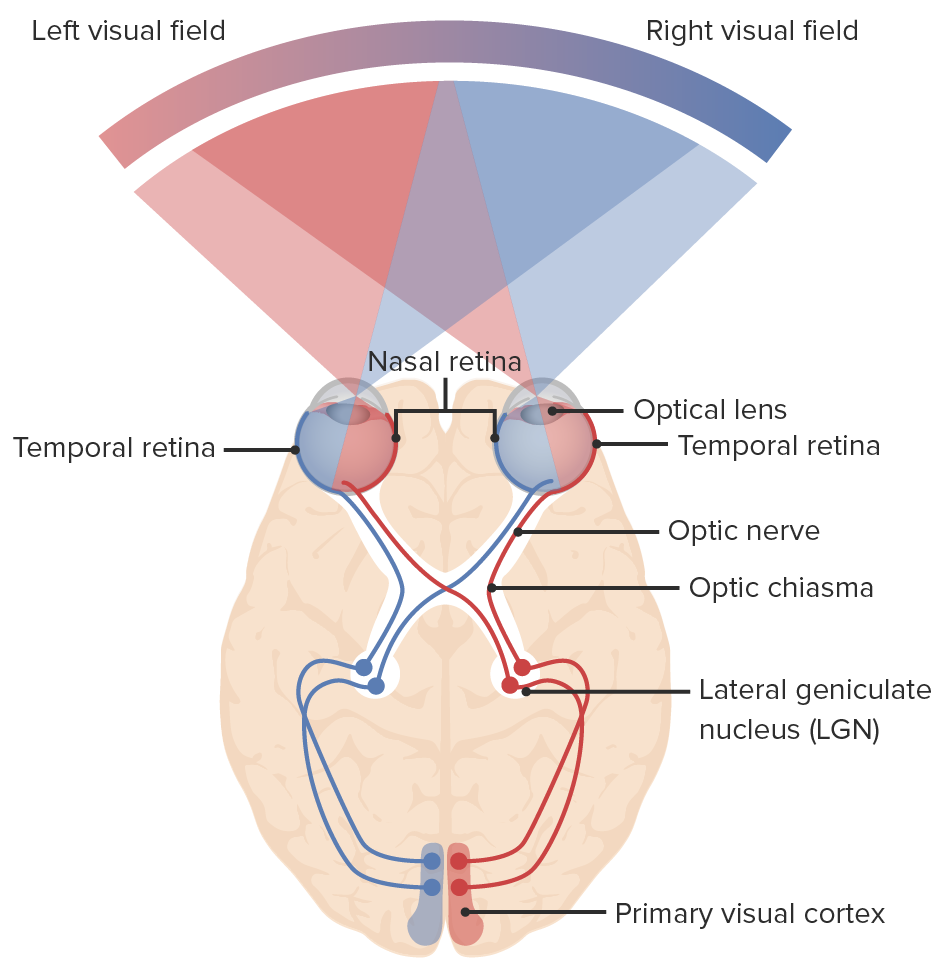
Glaucoma, a group of neurological disorders, can damage the optic nerve, responsible for transmitting light signals from our eyes to the brain for vision. This damage leads to visual field loss, and if not treated, can result in irreversible blindness. Glaucoma ranks as one of the leading causes of blindness globally, following cataracts. Understanding the significance of early detection and treatment is paramount in preventing glaucoma-related damage. Once glaucoma causes visual field loss, it becomes difficult to reverse the damage, potentially leading to blindness.
Who is at risk for Glaucoma?
Glaucoma is a condition that can affect individuals of all races and age groups. Certain factors can increase the likelihood of developing glaucoma, such as being African-American, having a family history of glaucoma, being diabetic, having high myopia (nearsightedness), or being over the age of 35. Numerous risk factors are associated with glaucoma, including advanced age, elevated intraocular pressure, family history, thin central corneal thickness, eye trauma, and a history of uveitis (eye inflammation), among others. The risk of glaucoma further increases after the age of 60.
Despite the availability of modern treatments, glaucoma remains a significant cause of preventable blindness. It is recommended that everyone undergo a glaucoma screening around the age of 35, followed by another screening at age 40. Individuals considered to be at higher risk, particularly those over the age of 60, should have their eye pressure checked annually or biennially. Early detection and treatment are crucial for preserving vision and enabling individuals to lead normal lives.
When assessing eye pressure, a normal range falls between 10 and 21 mmHg (individualized pressures may be considered for personalized therapy). However, in patients with glaucoma, the pressure can exceed 21 mmHg, depending on the specific type of glaucoma. It’s important to note that elevated blood pressure can further elevate eye pressure, posing an even greater risk to vision. Additionally, it should be noted that optic nerve damage and vision loss can occur in patients with normal eye pressure, a condition known as normal-tension glaucoma.
Types of Glaucoma
Glaucoma encompasses various types. The prevalent type in the United States is Open Angle Glaucoma, which develops slowly over years, usually without pain. It affects the general population and becomes more common with age. Early detection necessitates specialized testing, emphasizing the importance of regular eye exams by specialists to safeguard your health and vision.
Other forms of glaucoma include Closed Angle, Normal Tension, and Neo-vascular Glaucoma. Additionally, there are rarer forms like Pseudoexfoliation, Uveitic, and Traumatic Glaucoma. Each type requires specific treatment tailored to the illness, its stage, and the patient’s circumstances.
Symptoms of Glaucoma
Symptoms of glaucoma may begin with painless blurry vision and peripheral vision loss, progressing to the loss of central vision (impairing the ability to see objects or people directly in front of us). Unfortunately, this vision loss is typically irreversible and, if left untreated, can result in blindness. Closed-angle Glaucoma, on the other hand, can manifest suddenly, accompanied by severe eye pain, blurred vision, eye redness, and potential nausea or vomiting.


Screening for Glaucoma
Glaucoma specialists, who have undergone additional fellowship training in accredited universities, are highly skilled ophthalmologists dedicated to treating glaucoma. They possess state-of-the-art tests and equipment to screen, detect, and treat this condition. The commonly employed tests include Tonometry, Ophthalmoscopy, Perimetry, and Gonioscopy. It is worth noting that glaucoma testing usually does not necessitate a dilated exam, but your doctor can still conduct a comprehensive anterior segment exam to ensure thorough evaluation. Let’s delve into each test in detail.
Tonometry: Tonometry is a method used to measure eye pressure by delicately pressing a tonometer against the eye after administering numbing drops. Although it is essential to monitor eye pressure regularly, it is important to note that it can vary throughout the day. Surprisingly, low pressures can still impact the optic nerves in certain cases, while high pressures may be tolerated in others. To ensure safety and accuracy, additional tests are usually performed alongside tonometry.
Ophthalmoscopy: Ophthalmoscopy is a technique employed to evaluate the shape and color of the optic nerve. By administering eye drops to dilate the pupil, an ophthalmoscope is utilized to amplify and illuminate the inner part of the eye. If the optic nerve displays signs of being cupped or lacks a healthy pink color, further tests will be conducted to gather more information and insights.
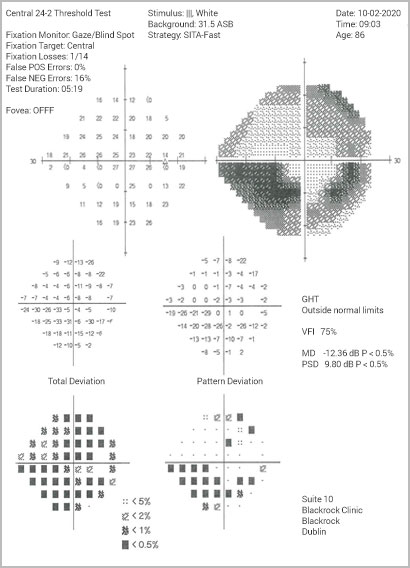
Perimetry: Perimetry is a specialized test designed to map the field of vision. During the examination, patients focus their gaze straight ahead into a white, bowl-shaped area. They are then prompted to indicate when they can perceive lights as they are introduced into their field of vision. This mapping process enables the doctor to detect any patterns of visual changes that may indicate the early stages of glaucoma.
Gonioscopy: Gonioscopy is a diagnostic procedure used to evaluate the angle where the iris meets the cornea, which helps determine whether it is open or closed. This assessment is valuable in identifying the presence of open-angle or narrow-angle glaucoma. Open-angle glaucoma accounts for approximately 90 percent of glaucoma cases. To effectively manage glaucoma, doctors employ three primary treatment options: medications, laser surgery, or filtration surgery. The primary goal is to lower intraocular pressure and sustain it at a healthy level to preserve vision.
Treatment for Glaucoma
At VSC, our expert cataract surgery and glaucoma surgery specialists can tailor surgical techniques to suit your specific needs. Our expert surgeons do a varity of advanced surgical procedures in the MIGSthat allow to preserve your vision speciality of like source of most up to date MIGS are mentioned below. Call us to find out which ones maybe right for you.
Medicines: Glaucoma medications are available in pill or eye drop form and aim to reduce fluid production or improve its drainage. Adherence to a consistent medication schedule, typically one to four times daily, is crucial. It’s important to be aware of potential side effects, and your doctor will work with you to find the most effective medication with minimal adverse reactions. It is essential to consult your doctor before discontinuing any medication and inform all healthcare providers about your current medications.
Laser Surgery: Laser surgery targets the drainage canal by applying a laser beam to the trabecular meshwork. Numbing eye drops are used during the procedure to enhance the drainage rate. Successful laser surgery can potentially reduce reliance on daily medications.
MIGS: Minimally Invasive Glaucoma Surgery (MIGS) represents a contemporary approach to glaucoma treatment. This technique employs small devices or implants to improve the eye’s natural drainage system, resulting in reduced intra-ocular pressure. MIGS procedures are typically performed alongside cataract surgery or as standalone procedures. They offer the advantage of being minimally invasive, leading to faster recovery times and lower risks compared to traditional glaucoma surgeries. MIGS provides an effective and safer option for managing glaucoma while preserving vision.
- iStent
- OMNI
- Hydrus
- Ahmed Valve Glaucoma Implant
- Barveldt Glaucoma Implant
and many more
Filtration Surgery: Filtration Surgery is recommended when medications and/or laser surgery fail to effectively control eye pressure. During this microscopic procedure, a new drainage channel is created to facilitate the drainage of aqueous fluid from the eye.